This systematic review and meta analysis assessed the association of breastfeeding with diabetes and hypertension amongst parents who breastfed for at least one year compared to less than one year. “Association of Maternal Lactation With Diabetes and Hypertension: A Systematic Review and Meta-analysis.”(1.)
Suzanne Sanders here, IBCLC for another article review.
Before we jump to the results, let’s dig in to the nitty gritty.
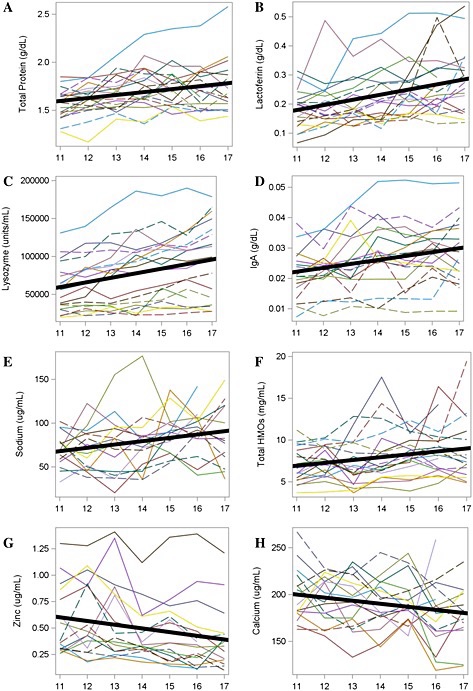
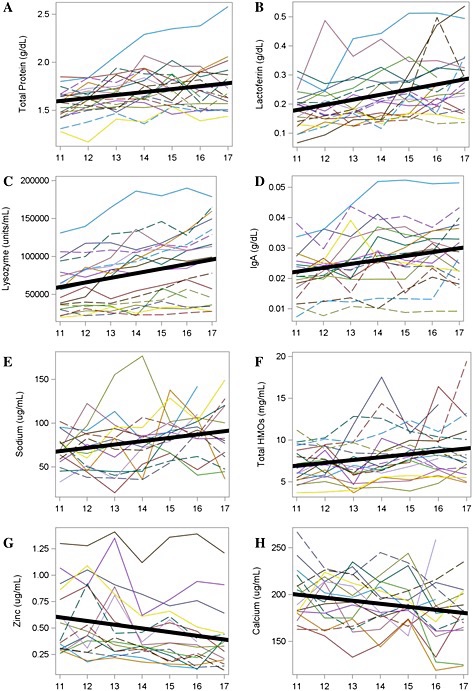
The systematic review encompasses 22 studies that look at breastfeeding in relation to hypertension and/or diabetes. They give brief overviews of many of these studies and it includes studies that compared different lengths of breastfeeding, not strictly 1 year.
For the meta analysis they found 4 studies that fit the criteria for breastfeeding and diabetes. Amongst these four studies, there was a total of 206,204 participants. 5 studies fit the criteria for breastfeeding and hypertension and their total participant count was 255,271 women.
The authors concluded from the meta analysis that “Breastfeeding for more than 12 months was associated with a relative risk reduction of 30% for diabetes (pooled odds ratio, 0.70 [95% CI, 0.62-0.78]; P < .001) and a relative risk reduction of 13% for hypertension (pooled odds ratio, 0.87 [95% CI, 0.78-0.97]; P = .01).” (1.)

What I am learning is a more appropriate title today. What exactly does it mean when the authors say a 30% RELATIVE RISK reduction or a 13% RELATIVE RISK reduction. Well I did some digging and it seems far more complex than something I can boil down to one short paragraph. If you want to sink your teeth into this concept – you could start by reading the sources that I found directly- then come back and share with us what you learn. So, to my understanding relative risk reduction tells you the difference between the control and the intervention. It does not tell you the risk for the control group and the risk for the intervention group OVERALL. That is the absolute risk. In order to get a good zoomed out picture of the situation, understanding both the relative risk and the absolute risk is important.
Definition of relative risk: “Relative risk is a ratio of the probability of an event occurring in the exposed group versus the probability of the event occurring in the non-exposed group.” (3.)
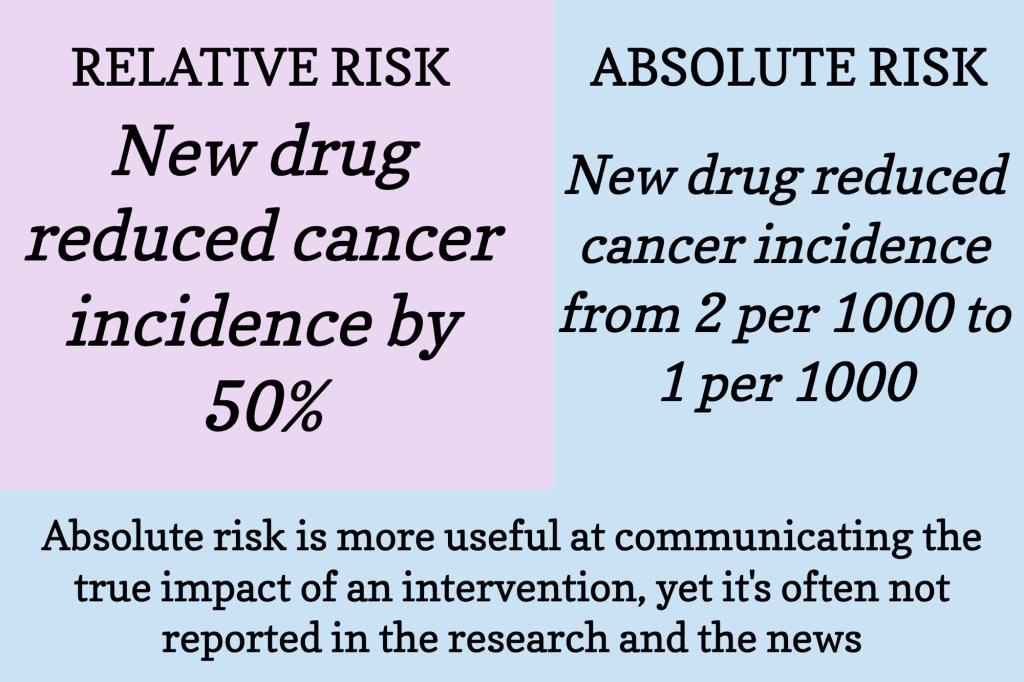
In the example above, the absolute risk gives you the overall risk of cancer incidence. While the relative risk is the difference between those two numbers. So, reducing the cancer incidence from 2/1000 to 1/1000 was a 50% decrease. But when you look at the overall risk of this cancer incidence, one question would be: is the medication worth the change in risk from 2 in 1000 people to 1 in 1000 people?
For our meta analysis we’re working with here, we know the relative risk reduction for diabetes/hypertension of breastfeeding for more than 12 months compared to breastfeeding for less than 12 months.
But, what is the absolute risk? I think the question that needs addressed before we can determine absolute risk is: What percentage of women acquire diabetes/hypertension in the years after they give birth (not during pregnancy or before child birth)?
If we had that knowledge then we could start to determine the overall risk these women have of getting diabetes/hypertension as it relates to breastfeeding.
This was a challenge, grasping relative risk. If you can share some knowledge, please drop a comment below and include your credentials (again, I don’t care if you’ve been in the research field for decades or this is your first time digging into this – giving us your credentials just helps everyone learn through the comments.)
Does ‘compared with breastfeeding for less than 12 months’ include those who did not initiate breastfeeding? I’d like to learn more about the length of time that people breastfed for when it was ‘less than 12 months”. Did the majority of them breastfeed for 3 months or 9 months or 2 weeks?
References:
2. Attia, Peter “Studying Studies: Part I – relative risk vs. absolute risk”. Updated 1/8/2018. Accessed 5/8/2025. https://peterattiamd.com/ns001/
3. Tenny S, Hoffman MR. Relative Risk. [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430824/
4. Calder, Robert A. “Statistical Thinking Part 2: Relative Risk, Absolute Risk, and Number Needed to Treat”. WMJ. 2024;123(4):324-327. Accessed 5/10/2025. https://wmjonline.org/123no4/calder/