“Your mental health is more important to me right now than any of this.” I overheard this exact quote multiple times in one lactation consultation. It was verbiage that I wrote down, thinking, I could use this phrase with my patients. The mother, with a history of depression and anxiety, has a newborn at home and has recently noticed the depression and anxiety seeping back into her life. She’s crying in the shower and having a hard time connecting with her baby. She has noticed that a big source of mental – and physical – pain is related to feedings. She has nipple damage and pain with latching, so she has also been pumping. She knows that breastmilk has some amazing nutrients for her baby. And, she is sinking into depression and finding it very difficult to connect with her little one.
Towards the end of this particular consult, after over an hour of evaluation and conversation, the IBCLC said “It sounds like mental health right now is our primary focus.” She then went on to have a conversation with her patient about different options for going forwards, all the while reiterating, multiple times, how mom’s mental health is ‘more important than any of this’ – indicating infant feedings.
This is such a hard place for a mother to find herself.
I think most parents in this situation ask themselves this question:
Do I prioritize my baby by offering him breastmilk so that he get those benefits at the expense of my mental health? Or, do I prioritize myself, stop breastfeeding and let my baby miss out on all of the benefits of breastmilk?
This is the wrong question.
A more appropriate question may be…
Is there a way I can improve my mental health and my breastfeeding experience?
– or –
If I am left with only two options: my mental health or breastmilk feeding; What is the right choice for my family (my baby AND myself)?
Let’s dive into the research behind both of these questions and see if we can encourage a parent in this position to look at their situation from a different point of view.
Question 1: Is there a way I can improve my mental health and my breastfeeding experience?
Here are some ideas that may help both mom’s mental health and their breastfeeding experience. Notice I said experience and not exclusive breastfeeding journey.
- Mom works with an appropriate provider to seek help for mental health. Maybe it’s counseling, maybe it’s medication, etc.
- Maybe we brainstorm a way for mom to get exercise and sleep and good nutrients into her daily schedule.
- Maybe they switch to exclusively pumping and bottle feeding.
- Maybe they switch to exclusively breastfeeding; if mom has low supply or baby cannot get the calories needed for growth then we top off with formula or donor milk after breastfeeding.
- Maybe they switch to formula feeding for calories, and breastfeed for comfort or for ‘desert’.
- Maybe she exclusively pumps for 24-48 hours while we do all of the things to get mom’s nipples healed, and then they go back to breastfeeding instead of pumping.
- Maybe they use a Supplemental Nursing System (SNS). Maybe they do not use SNS.
- Maybe they breastfeed, but switch one feeding every night to a bottle. Partner gives baby the bottle and mom gets an uninterrupted 4-8 hours of sleep. She may sacrifice breastmilk production, but it may be worth it if Mom’s mental health improves and we keep close tabs on baby’s weight gain.
- Maybe mom weans and they use donor human milk instead.
Here is some information to remind parents that even partial breast milk feeding has some amazing value:
Jump to this table from the American Academy of Pediatrics Breastfeeding and the Use of Human Milk policy statement from 2022 Table 2 (1.)
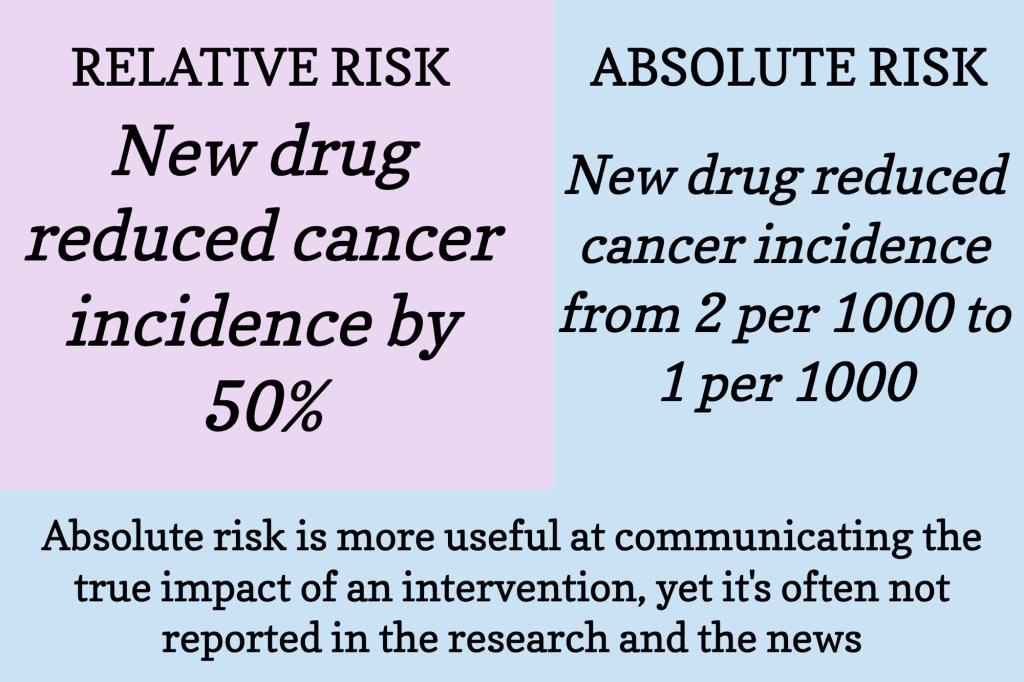
Seriously, jump to that website, glance at the chart, then come right back. Let me give you one example: Ever breastfeeding vs. never breastfeeding reduces the risk of otitis media (ear infection) by 33%. More vs. less breastfeeding reduce the risk of otitis media by 33%. Exclusive breastfeeding for 6 months reduces risk of ear infection by 43% compared to no breastfeeding at all (1.). This is a great example of how partial breastfeeding is STILL WORTH IT if we can improve mom’s mental health while we are at it.
Question 2: If I am left with only two options: my mental health or breastmilk feeding. What is the right choice for my family (my baby AND myself)?
There’s no doubt that breastmilk offers value to both mom and baby that they are not able to get with formula. That leaves us with the question: does the value (benefits) of breastmilk outweigh the risk of a maternal mental health disorder?
Jump to this policy statement from the American Academy of Pediatrics (2.) and go to the second section titled Impact on the Infant Dyad and Family.
Here’s a brief overview – Untreated maternal perinatal depression can lead to:
- infant at risk for toxic stress and its consequences – it can impact infants social-emotional development, including:
- Impaired social interaction
- Delays in language, cognitive, and social-emotional development
- Untreated PPD can lead to impaired parent-child interaction
- Immediate impairment of PPD can…
- hinder bonding, reciprocal interaction, and healthy attachment;
- distort perception of the infant’s behavior
- cause the mother to be less sensitive and attuned, indifferent, or more controlling
- impair the mother’s attention to, and judgment for, health and safety.
An original investigation published in JAMA Psychiatry in 2018 (3.) looked at postnatal depression in relation to two outcomes: (1) the trajectory of later EPDS scores, up to 11 years postpartum, and (2) child outcomes, up to 18 years old. When the children were 3.5 years old they looked at behavioral problems. At 16 years old math scores were assessed from a national public exam taken at the end of high school in the UK. When the children were 18 years old depression was assessed using a self-administered computerized interview.
They found that persistent and severe postnatal depression substantially raises the risk for adverse outcome on all child measures: the behavioral assessment, the math scores, and child’s depression at 18 years of age. They also noted that women with persistent postnatal depression showed elevated depressive symptoms up to 11 years after childbirth. Peristent and severe meant that the women had an EPDS score of 17 or higher at both 2 months postpartum and 8 months postpartum.
If a mom comes to this question, breastmilk OR mental health. I think it is important that we educate them on what is currently known about the value of breastmilk for both mom and baby as well as the benefits of positive maternal mental health. This way, our families can make an informed decision based on their specific situation.
To circle back around, mom’s mental health is very important to both herself AND her baby. Can we, as lactation professionals, use this data to encourage parents to prioritize their mental health and, just maybe, reframe their question?
RESOURCES